Most filers who received government subsidies to buy Obamacare plans had to pay money back to the IRS this year, according to an H&R Block analysis released Monday that looks at the health law’s first full tax season.
The tax-prep giant studied its own massive customer base and concluded that two-thirds of its filers who got subsidies from Obamacare were overpaid during the course of the year, and owed money back to the IRS on the April 15 deadline.
They repaid $729 on average, cutting the average refund by about a third.
Under the original terms of the Affordable Care Act they would have been capped at repayments of just $250, but Congress went back and lifted those caps, ensuring that the government could “claw back” most of the overpayments, and saving billions of dollars that have gone to other government priorities.
This tax season marked the first time the IRS has had to enforce its part of Obamacare — the tax penalties levied on those who lacked insurance, and the tax subsidies paid to Americans who qualified for help in buying plans.
Up to 7.5 million people got subsidies in 2014 based on their expected incomes, and had to use their tax forms to reconcile those projects with their actual income.
H&R Block said two-thirds of its filers were overpaid, but a quarter actually overestimated their earnings in 2014 and got more money back from the IRS on their taxes — tacking on an average of $425 to their refunds. The tax-preparation company said 13 percent of filers got their income estimates spot on.
“Our figures highlight the importance of estimating income as accurately as possible when applying for premium tax credits and notifying the marketplace with any life changes that impact annual household income or size,” said Mark Ciaramitaro, vice president of H&R Block health care and tax services.
Additionally, filers now face a tax penalty for failing to hold health insurance. For 2014, the penalty was $95 or 1 percent of household income over the filing threshold.
H&R Block also said the average penalty this season totaled $178, or nearly double the baseline $95, which some filers may have erroneously believed to be a flat fee.
The penalty for lacking coverage this year is $325 or 2 percent of income, rising to $695 or 2.5 percent of income in 2016.
Trying to match incomes and Obamacare subsidies has been a source of heated debate on Capitol Hill, and has proved to be tricky for many consumers.
SEE ALSO: David Vitter wants to subpoena D.C. exchange; Move ratchets up Obamacare fight
“If you’re a person who is a waitress or worked for a landscape company and you’re asked how much money you’re going to make, you’re really just throwing a dart at the board,” said Timothy Jost, a law professor at Washington and Lee University who closely tracks the health law.
The Affordable Care Act of 2010 initially capped the subsidy repayments at $250 for individual filers and $400 for non-individual filers, although those who made over 400 percent of the federal poverty level — and would no longer qualify for subsidies — had to pay all of the money back.
The caps were designed to make Obamacare more attractive to Americans using it for the first time.
But congressional Republicans pushed to raise the caps — twice — as part of bipartisan initiatives.
First, in 2010, as part of the annual “doc fix” to stave off cuts to Medicare reimbursements, and then again in 2011 to pay for the repeal of Obamacare’s unpopular “1099” provision, which would have required businesses to fill out a tax form every time they paid a vendor $600 or more.
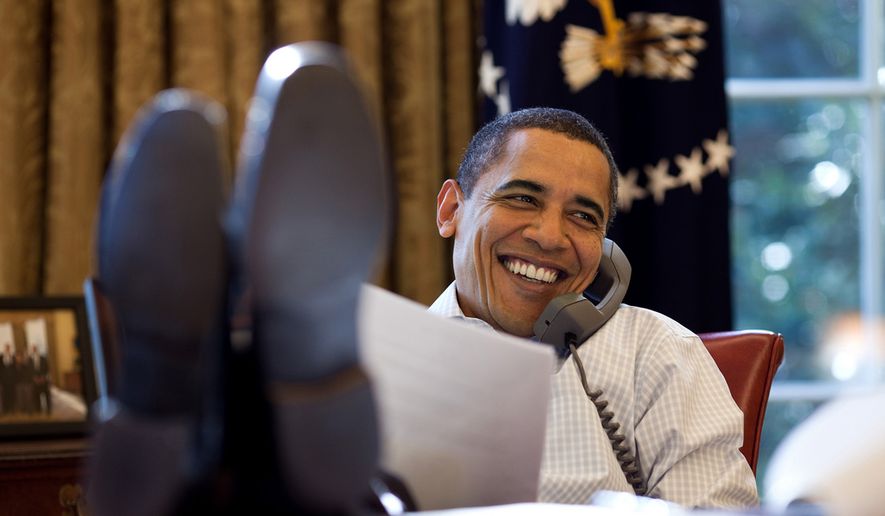
President Obama signed the changes into law even as Democrats complained that lifting the caps amount to a tax increase on low- and middle-income Americans.
Now, an individual who makes 200-300 percent of poverty would have to pay back up to $750, and those earning 300-400 percent would pay up to $1,250. For families, the corresponding maximums are $1,500 and $2,500.
Mr. Jost said H&R Block’s data suggests raising the caps had a dramatic effect, and that it might have been smarter to start with lower caps in the first years of Obamacare’s implementation, as customers get used to the law.
• Tom Howell Jr. can be reached at thowell@washingtontimes.com.



Please read our comment policy before commenting.